What Women (And Men) Should Know About Hormone Replacement Therapy
Bio-identical hormones have gained a lot of attention in recent years for managing aging-related symptoms caused by hormonal decline, but many questions and myths still surround the treatment. Our in-house Medical Director, Dr. Briggs, outlines the latest medical research about hormone replacement therapy and answers our client's most common questions.
1. What are Hormones?
Hormones are biological molecules produced in certain tissues called endocrine organs (for examples: Thyroid, Adrenal Glands, Ovaries and Testicles). They are able to influence other cells control bodily functions at a distance from where they are produced through transportation in the blood.
2. What happens to Hormones as we age?
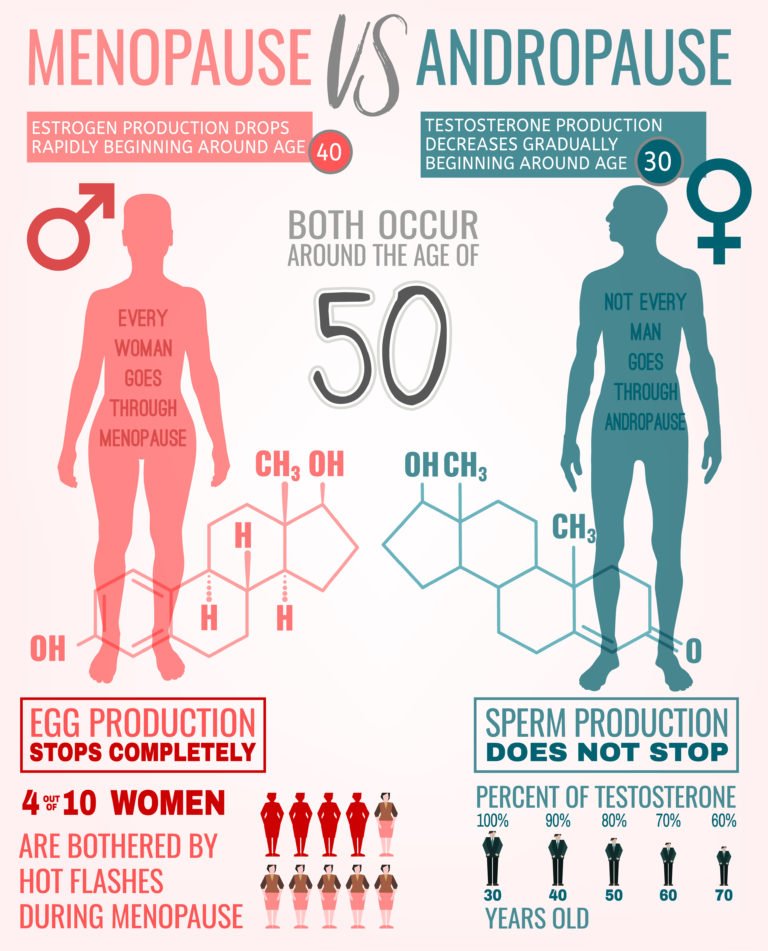
Generally, hormone levels decrease with age. Usually this is gradual, but it can occur quite suddenly such as when a woman reaches menopause (or has her uterus and ovaries removed) and her estrogen and progesterone production ceases abruptly.
This is made worse by the fact that hormone receptors also become more resistant with age (ex. Insulin Resistance). In other cases, hormone levels increase over time. This often occurs with Cortisol, a fight or flight response hormone which can have negative effects on the musculoskeletal, gastrointestinal, immunological and reproductive systems, if it is chronically elevated.
3. What is Hormone Replacement Therapy?
Hormone replacement therapy (HRT) is often used to treat the acute symptoms of menopause that 75% of women experience (hot flashes, night sweats, anxiety, depression, fatigue, insomnia and weight gain) in their early 50s. HRT not only can be used to treat the acute symptoms of menopause but it is believed to have a positive effect on women’s skin, hair, urethra (to prevent/treat recurrent bladder infections and urinary incontinence) and vaginal health (preventing dryness and painful intercourse).
In addition, many studies have demonstrated an association between HRT and reduced rates of cardiovascular disease (heart attacks, strokes and mini-strokes), osteoporosis, Alzheimer’s dementia, colorectal cancer, and macular generation in those taking HRT. The most common HRT offered to women is Premarin (a combination of mostly synthetic Estrogens) and Provera [Medroxy-Progesterone Acetate-MPA]) which is a synthetic Progesterone.
Autoimmune diseases of the thyroid gland (Hashimotos Thyroiditis and treated Graves Disease) often lead to hypothyroidism requiring treatment with thyroid hormone or Synthroid by family physicians.
"The most common symptoms of a low functioning thyroid (or due to under-treatment of a thyroid disorder) include dry skin, dry hair, hair loss, decreased energy, decreased mood, foggy thinking, aches and pains, difficulty “getting going” in the morning, constipation, loss of the outer 1/3 of the eyebrows, weight gain, cold intolerance and nail changes."
Because thyroid controls cellular metabolic activity (and therefore the Basal Metabolic Rate), adequate thyroid hormone is required to help people maintain their weight and feel and function well. HRT, when indicated by blood test results and guided by a patient’s symptoms, often includes prescribing thyroid hormone.
4. Why does Hormone Replacement therapy have a bad name?
Unfortunately, HRT has received a bad reputation due to the results of the Women’s Health Initiative (WHI). The study recruited women aged 50-79 years of age; they were placed on artificial estrogen and progesterone (Premarin and Provera). The study was stopped 2 years early, on May 31, 2002 because early results indicated a 29% increase in the risk for coronary heart disease. For women on the placebo arm of the trial (no HRT), the risk of a coronary event was about 30 women per 10,000 per year. If you were on hormone replacement therapy (HRT), this increased to 37 women per 10,000 per year. That's a 29% increase in risk. There was a 41% increase in risk for stroke.
This represented 21 women per 10,000 per year in the placebo group vs 29 women per 10,000 per year in the HRT group. The same was true of breast cancer, a 26% increase in the risk of breast cancer was found in the treatment group; the difference being 30 women per 10,000 per year in the placebo group and 38 women per 10,000 in the treatment group. However, the results also demonstrated a decrease in the risk of colorectal cancer that amounted to 37% and also a 34% decrease in the risk for hip fracture[i].
Now a key point to remember is that older women were enrolled in the study and started on HRT than most physicians would consider initiating treatment for (women greater than age 60). These women likely had other risk factors such as smoking, family history, high blood pressure, or increased cholesterol. In fact, later analysis of WHI data showed these younger women had an absolute risk of 12 adverse events per 10 000 women — less than a third of the risk of adverse events noted among women aged 70 to 79 — as well as fewer cancers, fractures and deaths from any cause compared to the placebo group[ii]. In my experience. Women do best when they begin HRT within 3-5 years of menopause. They can then remain on HRT indefinitely, or as long as they wish to prevent disease.
Another point to note is that, synthetic Progesterone (known as Progestins) as used in the WHI, are associated with an increased risk of breast cancer whereas natural Progesterone is associated with a reduced risk of breast cancer[iii]. Regardless, due to negative press from the WHI, the use of the HRT plummeted by as much as 80% following the release of the preliminary findings[iv]. A study published in 2013 estimated that as many as 91 610 American women died prematurely between 2002 and 2012 as a result of avoiding estrogen therapy[v].
5. What is the difference of Bio-identical Hormone Replacement Therapy (BHRT)?
Synthetic hormones differ in terms of molecular (structural) configuration than our own hormones. Therefore, synthetic hormones often vary in their ability to activate cellular proteins (receptors) as do our natural hormones. In addition, they often cause unwanted or unexpected side-effects (for example, Progestin effect in increasing the likelihood of breast cancer). Pharmaceutical companies develop and market synthetic hormones because they are able to patent them and make greater profit. Unless they develop a novel drug delivery system (a patch or micronized progesterone), pharmaceutical companies cannot patent natural hormones.
Most physicians and Nurse Practitioners have been trained only to prescribe synthetic hormones. Bio-identical Hormones are generally created by specialized compounding pharmacies from plant-based sources to be molecularly identical to natural hormones. These products can be creams, gels, lozenges, troches, capsules, pills, suppositories or even injections. They must be prescribed by physicians or nurse practitioners just like any other medication. Clinicians determine dosages depending on a patient’s symptoms and generally blood values, which must be regularly checked. The symptoms of too much or too little a dose of bio-identical hormones are the same as would be expected with a patient’s own natural hormones (ie. PMS symptoms in a perimenopausal women indicating higher levels of estradiol [estrogen]).
6. Who needs Bio-identical Hormone Replacement Therapy?BHRT can rapidly relieve most of the acute symptoms of menopause (hot flashes, night sweats, anxiety, depression, fatigue, and insomnia) within a few days of initiating treatment. In addition, estradiol treatment also improves aesthetics (hair and skin), and it can be helpful to prevent or improve recurrent bladder infections (60% reduction), urinary incontinence, vaginal dryness and painful intercourse. Testosterone therapy can improve exercise tolerance, muscle mass and libido.
Disease prevention is where hormone replacement therapy holds its greatest promise. Meta-analyses of polled studies have demonstrated that Hormone Replacement Therapy is associated with a 39% reduction in all-cause death compared to control (no HRT) groups, if initiated within a few years of menopause[vi]. It improves a broad spectrum of cardiovascular biomarkers (including cholesterol, insulin, nitric oxide and homocysteine levels)[vii]. A total of 48 470 healthy postmenopausal nurses aged 30-63 years in the Nurses’ Health Study were followed for 10 years to compare the incidence of cardiovascular disease and death among women taking estrogen and those not on hormone replacement therapy. The findings were that healthy postmenopausal women on estrogen therapy experienced a 44% reduced risk of major coronary disease compared to women not on estrogen (RR=0.56, CI: 0.40-0.80). remember, the WHI did also demonstrate a significant reduction in risk of colorectal cancer that amounted to 37% and also a 34% decrease in the risk for hip fracture[viii]. Another study observed a 30% reduction in Alzheimer’s Disease risk in Hormone Therapy users who initiated treatment within 5 years after menopause. This reduction was greater with sustained use of 10 years or more[ix]. Finally, the risk posed by artificial progesterone (progestins) is reversed when natural progesterone is used as part of the hormone therapy regime instead.
Therefore, newly menopausal women who wish to increase their health span and life span should strongly consider BHRT. Similarly, for those who are suffering from the acute effects of menopause and/or who want to preserve their aesthetics and sexual health are strongly encouraged to seek a consultation with a clinician providing this service. Younger women suffering from Polycystic Ovarian Syndrome or perimenopause are also encouraged to seek a consultation.
7. Are men candidates for BHRT?
As with women, Testosterone levels in men generally decrease with age.
"Typical symptoms experienced by men include decreased mood, grumpiness and irritability, decreased memory, weight gain (increased belly fat), decreased muscle mass, decreased exercise tolerance, decreased libido, decreased morning erections, and difficulty attaining and maintaining erections. In addition, low levels of testosterone can cause anemia and even osteoporosis[x]."
Men who suffer from these symptoms might be good candidates for Testosterone Replacement Therapy (TRT) depending on their blood work (Free Testosterone levels). Testosterone preparations are typically cream and occasionally injections; oral preparations are never used. Men who intend to have more children are encouraged to take subcutaneous HCG to ensure their sperm count is maintained while taking TRT. Despite extensive research on the issue, Testosterone has not been demonstrated to play a role in causing Prostate cancer.
8. Who shouldn’t take Hormone Replacement Therapy?
BHRT and HRT are not recommended in specific cases. Those women who have been diagnosed with breast cancer within the last 5 years should avoid estrogen, and testosterone therapy. Women beyond 5 years of breast cancer treatment are generally ok to have BHRT as are women who carry the BRCA I and II genes, which place them at greater risk for breast and other gynecologic cancers. Men who have been diagnosed with Prostate cancer, likewise should not be placed on Testosterone Replacement Therapy. It is important to understand that no studies have demonstrated that testosterone and estradiol (the natural or bio-identical forms) have not been shown to cause Prostate Cancer in men or Breast Cancer in women.
There are a number of congenital (inherited) and acquired clotting disorders; these include Leiden factor V, Antithrombin and prothrombin abnormalities, antiphospholipid syndrome (lupus anticoagulants), protein C and protein S deficiencies, and a few less common other disorders. For patients with these disorders, transdermal (cream or patches) estrogen preparations are safer.
9. Who should come in for a BHRT Consultation?
After reading this you believe you might be a good candidate for BHRT, please phone and make an appointment for a consultation.
[i]https://www.medscape.org/viewarticle/445476_5?src=ppc_google_rlsa_mscp_ed_md_ca-int&gclid=Cj0KCQjwg73kBRDVARIsAF-kEH8WU3TGJvJwcHupUGZBRnCN_pD138Cv2NTYTNc07tMCbbqVfKw1JXwaAqEAEALw_wcB[ii]
https://cmajnews.com/2017/04/12/landmark-trial-overstated-hrt-risk-for-younger-women-109-5421/[iii]
https://cmajnews.com/2017/04/12/landmark-trial-overstated-hrt-risk-for-younger-women-109-5421/[v]
Ibid.[viii]
https://www.medscape.org/viewarticle/445476_5?src=ppc_google_rlsa_mscp_ed_md_ca-int&gclid=Cj0KCQjwg73kBRDVARIsAF-kEH8WU3TGJvJwcHupUGZBRnCN_pD138Cv2NTYTNc07tMCbbqVfKw1JXwaAqEAEALw_wcB[ix]